INTRODUCTION
On behalf of the members, employees, consultants, volunteers and years of alumni, we welcome you to the Atlanta CV Drum & Bugle Corps (the “Corps”). We hope you enjoy a long and successful career teaching the young people who choose to be members of our corps.
This Physical Safety Guidelines policy is designed to assist you, members, administration and other staff members adhere to in order to maintain the health, safety and wellbeing of all who participate in our corps. Topics include roles and responsibilities, identifying and treatment of concussions, hydration, heat index, protocols for lightning as well as medical conditions that are common with our activity.
1 DEFINITIONS
- Health Staff: includes, but not limited to; athletic trainer, nurse, physician, physician’s assistant, nurse practitioner (when applicable)
- Administrative Staff: Executive Corps Director, Assistant Corps Director, Marketing Director, Operations, Logistics, Treasurer, Secretary
- Instructional Staff: Caption Heads, Technical Staff
2 ROLES AND RESPONSIBILITIES
All Staff:
- Safety should be at the forefront of everything we do.
- All staff are required to read and understand the Atlanta CV Drum & Bugle Corps Health Procedures annually.
Instructional Staff:
- Should guide or assist members to Health Staff when an actual or suspected medical/psychological issue or injury is identified.
Health Staff:
- Shall be certified in first aid and basic CPR with AED training.
- Primary objective is the health and safety of the corps members and staff.
- Will have the final decision-making authority regarding members’ participation in activities.
- Will not attempt procedures that are out of their scope of practice.
Administration Staff:
- Shall be certified in first aid, basic CPR and AED.
- In the absence of health staff, will have the final decision-making authority regarding members’ participation in activities.
3 CONCUSSION PROTOCOL
Signs and Symptoms of a Concussion:
| Cognitive Symptoms | Physical Symptoms | Emotional Symptoms |
| Poor Attention/Concentration | Headaches | Nervousness/Anxiety |
| Problems Remembering | Vacant Stare | Sad |
| Difficulty Following Conversation | Appears Dazed or Stunned | Irritability |
| Answers Questions Slowly | Dizziness | Personality Changes |
| Asks Same Question Repeatedly | Clumsiness/Balance Problems | Plays Less |
| Mentally Foggy | Fuzzy/Blurry Vision | |
| Sleeps More or Less than Usual | ||
| Appears Fatigued, Tired or Sleepy | ||
| Vomiting/Nausea |
- Staff will immediately inform the health staff of any member that sustains an injury during rehearsal that involves trauma to the head.
- The Health Staff will obtain injury details and assess the member. If symptoms are noted by the health staff, then the member will be excluded from all participation, until such time as the member is medically cleared to return to participation. If the member is under 18, the Health Staff will contact the parents, guardian or significant other directly within 24 hours.
- The Health Staff will notify the Executive Director, Assistant Director, Operations Administration or other appropriate staff and include the status of concussed members.
- If the member is taken to an urgent care or emergency room, the member will be accompanied by Health Staff. The member will then need to follow-up with the Health Staff as well as a licensed provider for retesting and medical re-evaluation before returning to physical activity, unless clear guidelines are given by the licensed provider during the initial visit. The member cannot participate in any performance or events until they have successfully completed the suggested full three-day progression and have remained symptom free. Return to rehearsal progression will be as follows:
Horns/Drumline
Day 1: Marching basics and stand still playing only.
Day 2: Marching basics, drill and stand still playing (no ensemble). Day 3: Full participation.
Color Guard
Day 1: Flag/Weapon basics, no tossing. Dance, not across the floors.
Day 2: Sectionals, spinning on the move. Dance across the floors (no ensemble). Day 3: Full participation.
Staff cannot override the decision of the Health Staff to exclude a marcher from participation.
4 LIGHTNING PROTOCOL
It is imperative that all personnel are aware of lightning hazards and the specific safety shelter for their venue. In the event of lightning during a rehearsal, precautions must be taken to ensure the safety of both members and spectators. In any event, the Admin/Health Staff, in conjunction with the acting director and/or public safety officials (i.e. police) if necessary will be responsible for monitoring inclement weather.
4.1 LIGHTNING DETECTION
Lightning awareness should be heightened at the first flash of lightning, clap of thunder and/or other criteria such as increasing winds or darkening skies, no matter how far away. The Admin/Health Staff is responsible for monitoring the progress of inclement weather by primarily using a weather app. The indicator for clearing the field or rehearsal with the weather app is 8 miles or less. In the event that members need to be removed from the rehearsal site, the Health Staff must notify the corps director who will then notify the staff. Once the staff has been notified, they must immediately comply, end rehearsal and move to a safe shelter.
4.2 SAFE SHELTER
Instructional staff should all be aware of the closest safe shelter to the rehearsal site and how long it takes to reach that shelter. A safe structure or location is defined as – “any sturdy, fully enclosed, substantial, and frequently inhabited building that has plumbing and/or electrical wiring that acts to electrically ground the structure”. Examples of locations that routinely DO NOT meet the criteria include:
- Baseball/Softball Dugouts
- Baseball/Softball “covered” Batting Cages
- Soccer Covered Bleachers
- Under Metal Bleachers
- Outside Storage Sheds; and/or
- Canopy/Awning/Tent
In the absence of a sturdy, fully enclosed, substantial, and frequently inhabited location as described above, a secondary structure such as a fully enclosed vehicle or tour bus with a hard metal roof, rubber tires, and completely closed windows can provide a measure of safety. Persons should not touch the sides of the vehicle!
Persons should avoid taking showers and using plumbing facilities (including indoor and outdoor pools, whirlpools, Jacuzzis, and hot tubs) and land-line telephones during a thunderstorm.
If no safe structure or location is within a reasonable distance, personnel should find a thick grove of small trees surrounded by taller trees or a dry ditch. Everyone should assume the “lightning-safe” position – a crouched position on the ground with the feet together, weight on the balls of the feet, head lowered, and ears covered. DO NOT LIE FLAT! Minimize the body’s surface area and minimize contact with the ground.
If unable to reach safe shelter, persons should stay away from the tallest trees or objects (i.e. light poles, flag poles, etc.), metal objects (i.e. fences, bleachers, etc.), individual trees, standing pools of water, and open fields. Persons should avoid being the highest object in an open field.
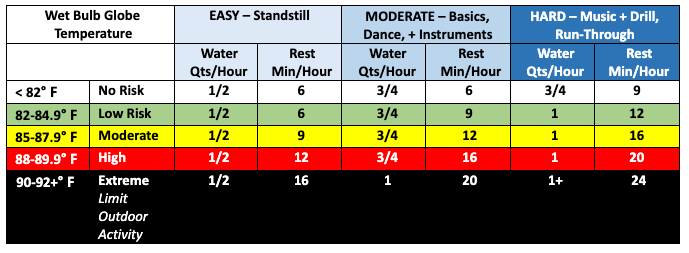
5 HEAT INDEX/HYDRATION PROTOCOL
High temperatures can present a dangerous situation for members and staff, but with reasonable precautions, those situations can be mitigated.
The administration staff must be consulted for the official temperature and the proper course of action for each day, and for each outdoor block held.
Whenever possible, the acting director and health staff should consult with each other as early as possible during a rehearsal or event day in order for all concerned parties to be notified of possible changes to schedules and locations appropriately.
The acting director will communicate any changes to the schedule of activities.
The following policies are the minimum standard for all outdoor activities within Atlanta CV. The use of more stringent policies is up to the director. Health staff and acting directors should collaborate prior to each rehearsal to discuss specific conditions and planned activities for rehearsal.
The acting director will communicate any change.
Staff should be aware of the signs of symptoms of dehydration:
| – Dry Mouth | – Thirst | – Irritability | – General Discomfort |
| – Headache | – Apathy | – Weakness | – Dizziness |
| – Cramps | – Chills | – Vomiting | – Nausea |
| – Head or Neck Heat Sensations | – Excessive Fatigue and/or Decreased Performance | ||
*If any of these signs or symptoms are observed, notify the administration staff immediately. Early detection of dehydration decreases the occurrence and severity of heat illness.
A staff member is designated to monitor heat when warm/hot and humid conditions are forecast. This person will have the authority to activate hydration protocols and mandatory rest periods. Heat index and Wet Bulb Globe Temperature will be monitored from weather apps or an appropriate WBGT device if available.
5.1 HEAT CRAMPS
Cramps that occur during exercise or physical activity.
5.1.1 TREATMENT
-
- Hydrate the member and replace sodium losses with a sports drink or other source of salt.
- Relax, stretch, and massage the involved muscle to reduce acute discomfort.
5.1.2 PREVENTION
-
- Adequate conditioning, acclimation, hydration, electrolyte replacement, and appropriate dietary practices.
5.2 HEAT EXHAUSTION
Inability to keep up with exercise due to intensity of effort and environmental heat factors.
5.2.1 SYMPTOMS
-
- High pulse rate and low blood pressure
- Extreme weakness
- Dehydration and electrolyte losses
- Coordination problems, fainting, lightheadedness
- Profuse sweating, paleness,“prickly heat” sensations
- Headache
- Abdominalcramps, nausea, vomiting, diarrhea
- Persistent muscle cramps
- Mild confusion which can quickly resolve with rest and cooling
5.2.2 TREATMENT
-
- Move members to shaded or air-conditioned areas to rest.
- Remove extra clothing or gear.
- Cool with cold water, fans, or cool towels, ice packs to neck, armpits, groin (replaced every 2-3 minutes).
- Lay with legs raised above the level of heart.
- Give members cool/cold fluids to drink if not vomiting.
- If symptoms do not improve within 30 minutes, call 911 or send members to hospital.
5.3 EXERTIONAL HEAT STROKE
High core body temperature along with organ dysfunction. The longer the body is at an elevated temperature, the more dangerous. Temperature is usually 104 degrees or above.
5.3.1 SYMPTOMS
-
- Disorientation, headache, irrational behavior, irritability, emotional instability, confusion, altered consciousness, coma, or seizure.
- Hyperventilation, dizziness, nausea, vomiting, diarrhea, weakness, profuse sweating, dehydration, dry mouth, thirst, muscle cramps, loss of muscle function, and ataxia.
5.3.2 TREATMENT
-
- Call 911, THIS IS A MEDICAL EMERGENCY!
- In the meantime, initiate cooling measures, “cool first, transport second”.
- Move members to shaded or air-conditioned areas to rest.
- Remove extra clothing or gear.
- If available, put in a tub with cold/ice water; place in a cold shower, douse with water from the hose.
- Cool with cold water and fans, or cool towels or ice packs to neck, armpits and groin (replaced every 2-3 minutes), lay with legs raised above the level of heart.
- Give members cool/cold fluids to drink if not vomiting.
- Cool until the member begins to shiver OR for 15-20 minutes of active cooling ORmedical help arrives.
SOURCES:
Statement: exertional Heat Illness, Binkley, H.M., Beckett, J., Casa, D.J., Kleiner, D.M., & Plummer, P.E. (2002)). National Athletic Trainers’ Association Position Journal of Athletic Training, 37(3), 329-343.
6 ASTHMA
Members diagnosed with asthma should have a rescue inhaler available during all rehearsals and performances. At NO time should a member not diagnosed with asthma make use of an inhaler. NO staff member will advise any member to take an inhaler that is not prescribed to them.
6.1 SYMPTOMS
Notify the health staff immediately if you notice the following:
- Significant increase in wheezing that you can hear
- Chest tightness
- Fast breathing
- Inability to speak in full sentences
- Uncontrolled cough
- Nasal flaring
6.2 TREATMENT
- Remove members from activity.
- Have members take their rescue inhaler.
- Assist members with nose breathing technique.
- Have the member take a deep breath through the nose and out the mouth.
- Raising their arms will help the lungs expand.
- Try to calm the member, panicking increases the respiration rate.
- Call 911 if no improvement is observed in 10 minutes.
7 ALLERGIES
Members who have been diagnosed with severe allergies should notify the health staff, directors, and any food preparers of the nature and severity of their allergies. Members requiring epinephrine auto-injector should have a minimum of one pen with them at all times.
7.1 SYMPTOMS
Hives, redness, difficulty breathing, wheezing, tongue swelling, feeling like my throat is closing.
7.2 TREATMENT
Health Staff Present:
- If a member is able to administer their own epinephrine auto-injector, the health staff will supervise proper administration.
- If a member is not able to administer their own epinephrine auto-injector, health staff will administer it for them, by injecting it in the mid/outside thigh. Health staff will then activate EMS for transportation to the ER for further treatment.
- Health staff will note the time the epinephrine auto-injector was administered, if available a second epinephrine auto-injector dose will be administered 15 minutes after the first injection.
- If a second epinephrine auto-injector is not available, health staff will provide the member with Benadryl.
- Upon EMS arrival, health staff will provide EMT/Paramedics with the administered epinephrine auto- injector(s) and time(s) of administration. If a member is under the age of 18, the member’s parents will be contacted directly. Health staff will accompany members to the hospital.
Health Staff is not Present:
- If a member is able to administer their own epinephrine auto-injector, instructional staff will assist if needed. If a member is unable, staff will administer it for them, by injecting it in the mid/outside thigh. Staff will then activate EMS for transportation to the ER for further treatment.
- Instructionalstaff will note the time the epinephrine auto-injector was administered.
- If available, a second epinephrine auto-injector will be administered 15 minutes after the first injection. If a second epinephrine auto-injector is not available, instructional staff will provide the member with Benadryl.
- Upon EMS arrival, instructional staff will provide EMT/Paramedics with the administered epinephrine auto-injector(s) and time(s) of administration. If a member is under the age of 18, the member’s parents will be contacted directly. Staff will accompany members to the hospital.
8 COMMON INJURIES
SPRAINS – Overstretching or tearing of the ligaments. Treat with ice, rest, wrap.
STRAINS – Overstretching or tearing of the muscle or tendon. Treat with ice, rest, wrap.
LOWER LEG PAIN/SHIN SPLINTS – Overuse. Treat with ice on breaks, medications, assess footwear. Refer for x – rays if needed.
FRACTURES – Broken bones. Treat initially with ice, elevation, immobilization if needed. Refer For X-rays.
PAIN/SORENESS – Treat with ice initially, then move to heat, gentle stretching, medication.
CRAMPS – Slowly stretch against the cramp, massage, consider electrolytes if heat is a factor.
SKIN RASHES – If itching, try Benadryl 50mg, try hydrocortisone cream. Urgent Care or ER if concerning.
ABRASIONS – Clean with tap water twice daily, antibiotic ointment, bandage, protect from sun.
LACERATIONS – Clean with tap water twice daily, antibiotic ointment, bandage, protect from sun for up to 6 months to prevent scarring.
REDNESS – Cellulitis (infection of skin) or infection of wound.
INFECTIONS – Redness, swelling, heat. Skin and wound infections require antibiotics.
GROIN PULL – Treat as sprain – ice, rest.
TESTICULAR PAIN – Initial treatment, ice, supportive underwear, refer to ER.
ABDOMINAL PAIN – This can be many things. If concerning, refer to ER.
VOMITING/DIARRHEA – Decrease food intake, encourage frequent small amounts of fluids and increase as tolerated. If significantly dehydrated, refer to ER.
SUICIDAL – Someone should stay with the person at all times, referdirectly to ER.
TYLENOL – Overdose can cause liver damage, limit to 3,000 mg per day (9 regular or 6 extra-strength pills per day).
IBUPROFEN – Overdose can cause kidney damage, can cause ulcers, limit to 3,200 mg per day (16 pills per day).
9 WHEN TO USE TELEMEDICINE, URGENT CARE OR EMERGENCY ROOM
TELEMEDICINE: Rashes, psychological(depression, anxiety), urinary tract infection.
URGENT CARE: Strains, sprains, lacerations, fractures, pain/soreness, skin infections, groin/muscle pulls – usually can perform x-rays.
EMERGENCY ROOM: Deformed fractures, complex/deep lacerations, concussions, suicidal, abdominal pain, severe vomiting/diarrhea with dehydration, testicular pain – when CT, MRI are needed.
Although rare, there are some situations where you will need to call 911 and activate the Emergency Medical Services (EMS). The following are medical emergencies:
- Anytime a marching member or member of staff has a loss of consciousness of any duration. While loss of consciousness is not required for a concussion to occur, it may indicate more serious brain injury.
- Seizure
- Increasing Sleepiness
- Worsening Headache
- Persistent Vomiting